Award-winning PDF software





Provider credentialing process flow Form: What You Should Know
Second, you need an attestation of competency by a qualified health care professional or physician (or both depending on your situation). Lastly, you need to be authorized to perform some functions. You will need to provide documentation (in the form of a medical certification) to get a medical exemption from an employer or hospital. You will need to provide documentation (in the form of a medical certification) to get a medical exemption from an employer or hospital. First, you will need to identify all medical providers who qualify for medical exemption. Step 1. Step: 1, Identify the Required Documents #2 Identify the Required Documents #3 Create an Authorization Form Step: 2, Identify the Required Documents #4 Create an Authorization Form #5 Attach the Required Medical Certification to the Authorization Form In the Attachments section of the Authorization Form, attach all three (3) documents, as shown in the list. The completed Authorization will be mailed to the employee/physician, stating whether the employee/physician is authorized to perform the function for which he/she is sought to demonstrate proficiency.” Attach the Required Medical Certification to the Authorization Form Step: 3, Attach the Requirement Documents Step: 4, Identify the Required Documents for the Relevant Position (The first step in credentialing) Step: 5, Identify Required Documents for the Specific Position (The second step in credentialing) Step: 6, Add Optional Documents of the Competencies (Steps 3 and 4). Step: 7, Evaluate the Competencies Step: 8, Create a Contract Next, you may decide whether to have an attestation of competency, a medical certificate, or additional documentation. If you do decide to have a medical certificate, you need to have written permission from your employer/hospital. Also, it is usually easier to use Attestation of Competency to become a Physician Assistant than it is to use a Medical Certificate. Credential Evaluation Process Step: 1: Evaluate the Competencies Step: 2, Create a Contract Step: 3: Attach Medical Certificate. Step.
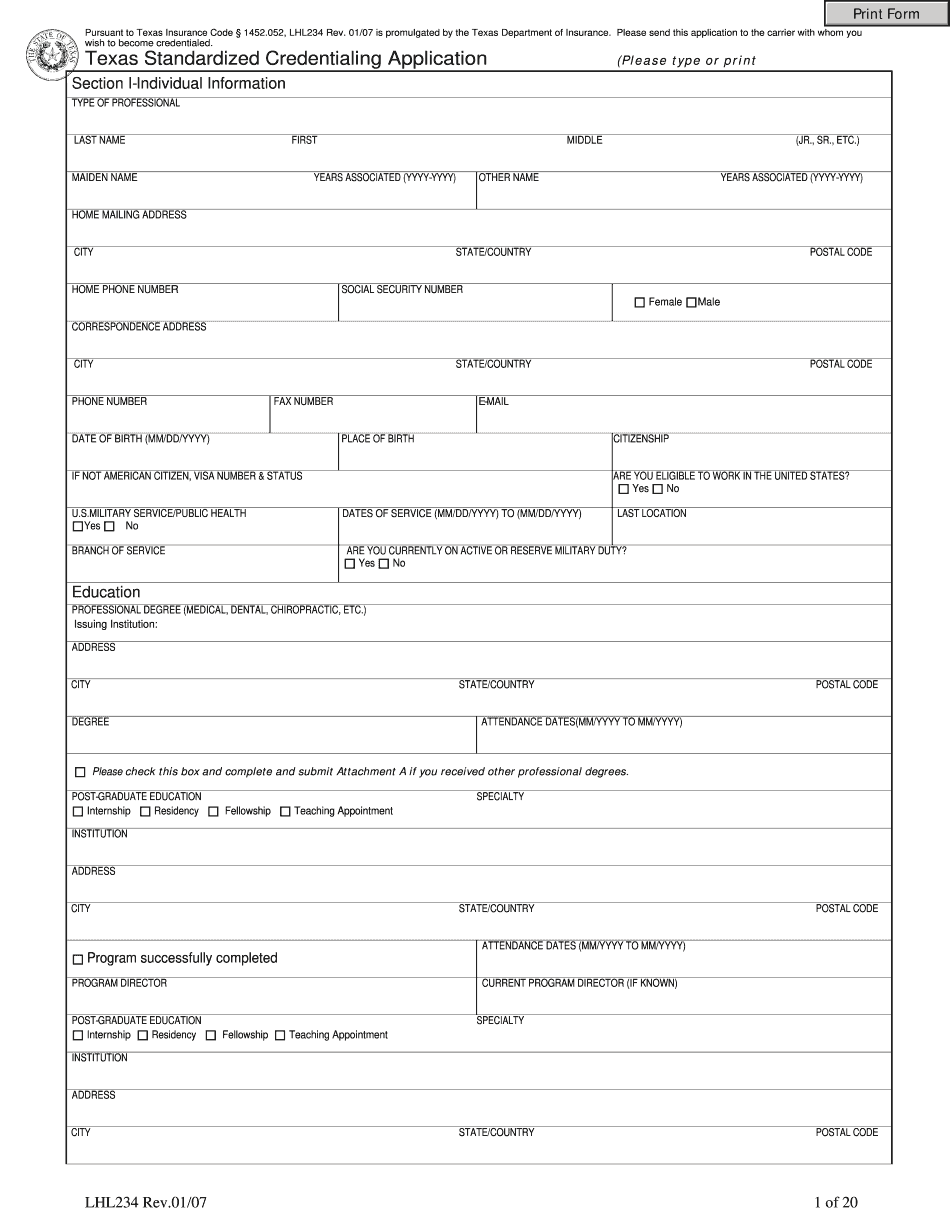
online solutions help you to manage your record administration along with raise the efficiency of the workflows. Stick to the fast guide to do TX Tdi Lhl234, steer clear of blunders along with furnish it in a timely manner:
How to complete any TX Tdi Lhl234 online: - On the site with all the document, click on Begin immediately along with complete for the editor.
- Use your indications to submit established track record areas.
- Add your own info and speak to data.
- Make sure that you enter correct details and numbers throughout suitable areas.
- Very carefully confirm the content of the form as well as grammar along with punctuational.
- Navigate to Support area when you have questions or perhaps handle our assistance team.
- Place an electronic digital unique in your TX Tdi Lhl234 by using Sign Device.
- After the form is fully gone, media Completed.
- Deliver the particular prepared document by way of electronic mail or facsimile, art print it out or perhaps reduce the gadget.
PDF editor permits you to help make changes to your TX Tdi Lhl234 from the internet connected gadget, personalize it based on your requirements, indicator this in electronic format and also disperse differently.